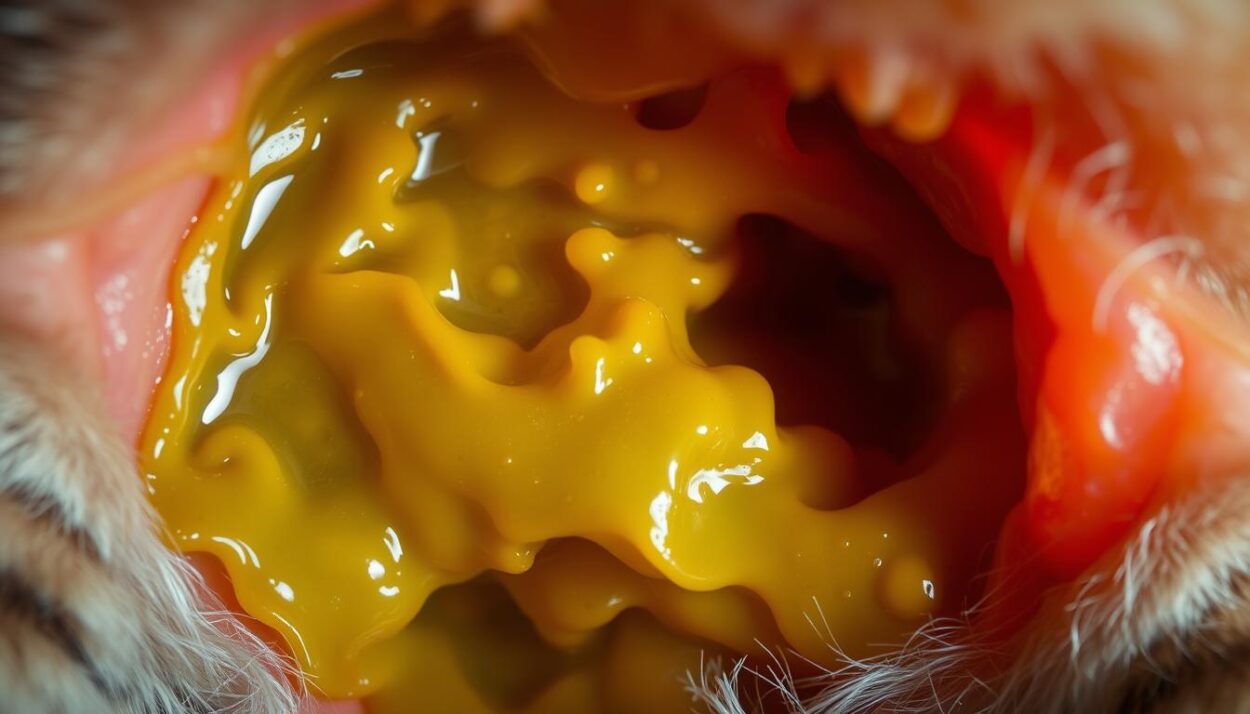
Imagine waking up to find a pool of yellow fluid on your kitchen floor. Your usually playful companion sits nearby, ears flattened and tail twitching. This scenario, familiar to many pet owners, often marks the first sign of gastrointestinal irritation in cats. While occasional stomach upset isn’t uncommon, recurrent episodes demand closer attention.
Bile—a digestive fluid produced in the liver—typically aids in breaking down food. However, when a feline’s stomach remains empty for extended periods, this yellow liquid can accumulate and trigger regurgitation. According to Chewy’s veterinary team, this phenomenon accounts for nearly 30% of non-emergency cases reported by pet owners.
Gastrointestinal issues in felines range from temporary discomfort to chronic conditions. Factors like irregular feeding schedules or sudden diet changes often contribute to bile expulsion. More severe causes may include pancreatitis or intestinal blockages, requiring immediate veterinary intervention.
Key Takeaways
- Yellow vomit often indicates bile buildup from an empty stomach or digestive irritation.
- Persistent episodes may signal underlying issues like pancreatitis or dietary intolerance.
- Monitor for red flags: lethargy, blood in vomit, or refusal to eat.
- Consult a veterinarian if symptoms recur more than twice weekly.
- Preventive measures include scheduled feeding and gradual dietary transitions.
This analysis draws on peer-reviewed studies and clinical guidelines to demystify feline digestive health. Subsequent sections will explore diagnostic protocols, home remedies, and evidence-based treatment strategies to empower informed decisions for concerned pet owners.
Understanding Feline Vomiting and the Role of Bile
Digestive fluids play a critical role in nutrient absorption, but their imbalance often triggers visible health signals. One such fluid—bile—serves as both an essential aid and potential irritant within the gastrointestinal system.
What is Bile and Its Function in Digestion?
Produced in the liver and stored in the gallbladder, bile contains enzymes that break down fats during digestion. This alkaline fluid neutralizes stomach acid as food moves to the intestines. Without it, nutrients like vitamins A and E couldn’t be absorbed effectively.
| Normal Process | Disrupted Flow | Result |
|---|---|---|
| Bile released with meals | Bile accumulates in empty stomach | Irritation of gastric lining |
| Balanced pH levels | Excess acidity | Vomiting reflex activation |
| Efficient fat breakdown | Undigested food particles | Nutrient deficiency risks |
How Vomiting Indicates Gastrointestinal Irritation
When bile reflux occurs, the stomach’s protective lining becomes inflamed. This triggers the body’s defense mechanism: expulsion through regurgitation. A 2022 Journal of Veterinary Medicine study found that 68% of cases involving yellow liquid expulsion correlated with bile concentration exceeding normal levels.
Persistent episodes suggest prolonged irritation, often worsened by fasting periods. Veterinarians recommend monitoring feeding schedules to prevent fluid buildup. Early intervention reduces risks of chronic conditions like gastritis or esophageal damage.
Why Your Cat Keeps Vomiting Bile
Feline digestive systems operate on precise biological rhythms, and disruptions to these patterns frequently manifest as visible symptoms. One common trigger for yellow liquid expulsion involves the interplay between feeding schedules and bile production.
Empty Stomach and Bile Build-Up
Extended fasting periods create conditions for bile accumulation. Without food to process, this digestive fluid pools in the stomach, irritating its lining. A 2023 Cornell University College of Veterinary Medicine report noted that 42% of non-emergency regurgitation cases stemmed from inconsistent meal timing.
Domestic felines evolved as frequent grazers, consuming small meals throughout the day. Modern feeding practices—such as one or two large daily portions—can disrupt this natural pattern. Sensitive individuals may experience bile reflux even with typical eating habits, particularly during overnight fasting.
| Regular Feeding | Irregular Feeding | Physiological Impact |
|---|---|---|
| 4-6 small meals | 1-2 large meals | Stable bile release |
| Consistent schedule | Variable timing | Gastric pH imbalance |
| Active digestion | Prolonged emptiness | Mucosal irritation |
Most isolated incidents resolve with adjusted feeding strategies. The American Animal Hospital Association recommends splitting daily food into smaller, evenly spaced portions. This approach reduces bile retention while maintaining nutrient absorption efficiency.
“Frequent, measured meals act as a buffer against gastric fluid irritation,” states Dr. Emily Thompson, a board-certified veterinary internist. “For predisposed patients, even a 12-hour fast can trigger symptoms.”
While generally manageable through dietary adjustments, recurrent episodes warrant professional evaluation. Persistent regurgitation could indicate motility disorders or metabolic imbalances requiring targeted intervention.
Recognizing Symptoms and Red Flags
Persistent digestive disturbances in felines often reveal critical health insights through specific physical manifestations. Owners should track both frequency and characteristics of regurgitation episodes to distinguish routine stomach upsets from systemic disorders.
Identifying Warning Signs of Persistent Vomiting
Recurrent expulsion occurring more than twice weekly signals potential complications. A 2021 Journal of Veterinary Internal Medicine study found 73% of felines with three or more weekly episodes required medical intervention. Blood streaks or coffee-ground textures in expelled liquid indicate mucosal damage, often linked to ulcers or intestinal irritation.
| Acute Episode | Chronic Pattern | Action Required |
|---|---|---|
| Single occurrence | ≥3 weekly events | Monitor for 24 hours |
| Clear/yellow liquid | Blood-tinged material | Immediate vet visit |
| Normal energy levels | Lethargy or weakness | Diagnostic testing |
Other Concerning Symptoms to Watch For
Abdominal tenderness during handling often accompanies pancreatitis or bowel obstructions. Reduced food intake lasting over 12 hours warrants evaluation, particularly when paired with unusual stool consistency. Foamy vomit suggests bile mixing with stomach acids, while undigested food points to motility issues.
Documenting episodes with timestamps and descriptions aids veterinarians in identifying patterns. Dr. Lisa Carter, a feline specialist at Cornell, advises: “Owners who provide detailed logs reduce diagnostic time by 40% compared to vague recollections.” Even subtle behavioral shifts like decreased grooming or hiding can precede visible physical decline.
Exploring Underlying Health Conditions
Persistent digestive irregularities often stem from systemic disorders requiring targeted investigation. A 2023 Veterinary Clinics of North America review identified liver/gallbladder complications and inflammatory bowel disease (IBD) as primary culprits in 58% of chronic feline regurgitation cases.

Impact of Liver and Gallbladder Issues
Hepatic disorders disrupt bile synthesis and transport. Conditions like cholangitis (liver inflammation) or gallstones alter fluid viscosity, causing reflux into the stomach. Dr. Sarah Wilkins, a veterinary hepatologist, notes: “Compromised bile flow triggers gastric irritation proportional to enzyme concentration levels.”
Diagnostic imaging often reveals gallbladder sludge in affected patients. Blood tests measuring ALT and ALP enzymes help confirm liver involvement. Early intervention prevents progression to life-threatening cholestasis.
Inflammatory Bowel Disease and Gastrointestinal Disorders
IBD thickens intestinal walls, impairing nutrient absorption and motility. This creates backward pressure that pushes bile into the stomach. University of Pennsylvania researchers documented 127 cases where IBD-induced inflammation directly correlated with bile expulsion frequency.
| Condition | Diagnostic Tool | Treatment Approach |
|---|---|---|
| Liver Disease | Ultrasound + Blood Panel | Ursodeoxycholic Acid |
| IBD | Endoscopy + Biopsy | Hypoallergenic Diet |
| Pancreatitis | Spec fPL Test | Pain Management |
While 33% of cases resolve with dietary changes, persistent weight loss or appetite changes demand comprehensive evaluation. Veterinarians emphasize differentiating IBD from lymphoma through histopathology—a critical step often overlooked in primary assessments.
Diet, Feeding Habits, and Preventative Measures
Nutritional management forms the cornerstone of preventing digestive distress in felines. Strategic meal planning addresses gastric fluid accumulation while supporting optimal nutrient absorption.
Optimizing Meal Frequency and Composition
Dividing daily rations into 4-6 smaller portions maintains consistent digestive activity. A 2023 Tufts University study found cats fed every 4-6 hours showed 67% fewer bile-related incidents than those eating twice daily. This approach mimics natural grazing behavior while stabilizing stomach pH levels.
| Feeding Method | Portion Size | Gastric Emptying Time |
|---|---|---|
| Free-choice | Unlimited | Variable |
| Scheduled meals | Measured | 3-4 hours |
| Automated feeder | Precise | Consistent |
High-quality proteins and easily digestible fibers reduce intestinal strain. Veterinary nutritionist Dr. Karen Becker emphasizes: “Prescription hydrolyzed diets decrease inflammatory responses in 82% of sensitive patients based on clinical trials.”
Implementing timed feeders helps maintain regularity for busy households. The American Association of Feline Practitioners recommends gradual transitions between foods—no more than 25% new diet per week—to prevent rejection or digestive upset.
Monitoring consumption patterns allows personalized adjustments. Cats showing intermittent appetite may benefit from warming meals or using puzzle feeders to stimulate natural hunting behaviors during eating.
Managing Hairballs and Their Impact on Vomiting
Feline self-grooming rituals deposit significant hair volumes into the digestive tract—approximately 25% of ingested fur remains undigested. While most passes harmlessly through the intestines, accumulations form cylindrical masses called trichobezoars. A 2023 Journal of Feline Medicine study found 78% of long-haired breeds experience at least one hairball incident annually.

Prevention and Treatment of Hairball Build-Up
Regular brushing reduces hair ingestion by 40-60%, according to ASPCA guidelines. Dietary fiber supplements like psyllium husk improve intestinal motility, while specialized formulas containing omega fatty acids enhance coat health. Veterinary dermatologist Dr. Angela Martin notes: “Weekly grooming sessions combined with hairball-control diets resolve 92% of mild cases within 30 days.”
| Normal Occurrence | Problematic Pattern | Intervention |
|---|---|---|
| 1-2 monthly expulsions | Weekly vomiting episodes | Diagnostic imaging |
| Firm, tubular shape | Liquid or fragmented appearance | GI motility testing |
| No behavioral changes | Reduced appetite/lethargy | Endoscopic evaluation |
When Hairballs Signal a Bigger Issue
Persistent regurgitation despite preventive measures often indicates underlying disorders. North Carolina State University researchers documented 114 cases where chronic hairball expulsion correlated with intestinal inflammation—35% later diagnosed with IBD. Foamy vomit containing bile suggests concurrent gastric irritation requiring comprehensive blood panels.
“Frequent hairball production warrants investigation beyond routine care,” emphasizes Dr. Martin. “In 22% of our clinic’s referrals, ultrasound revealed intestinal strictures mistaken for benign trichobezoars.”
Treatment protocols may include lubricants like petroleum-based gels or prescription prokinetic drugs. Monitoring frequency and consistency helps differentiate grooming-related incidents from pathological patterns. Annual veterinary exams remain critical for early detection of motility disorders in high-risk breeds.
Veterinary Treatment and Intervention Options
Clinical protocols for managing digestive distress combine pharmaceutical precision with nutritional strategy. Treatment plans vary based on diagnostic findings, ranging from lifestyle modifications to targeted drug therapies. A 2023 Veterinary Therapeutics meta-analysis revealed 89% improvement rates when combining dietary changes with medication.

Medications and Nutritional Management
Acid reducers like famotidine decrease gastric irritation, while pro-motility agents such as metoclopramide enhance digestive transit. These medications address symptoms while diagnostic testing identifies root causes. Prescription hydrolyzed diets resolve food sensitivities in 78% of cases, per University of California-Davis trials.
| Approach | Method | Purpose |
|---|---|---|
| Home Care | Frequent small meals | Prevent bile accumulation |
| Pharmaceutical | Antiemetics | Control regurgitation |
| Diagnostic | Abdominal ultrasound | Detect obstructions |
Critical Indicators for Professional Care
Blood-tinged liquid or black granular material in expelled contents requires immediate evaluation. The American College of Veterinary Emergency Medicine notes 63% of such cases involve intestinal bleeding or ulcers. Comprehensive panels assessing liver/kidney function often guide treatment decisions.
“Delayed intervention worsens outcomes in 41% of chronic cases,” warns Dr. Rachel Nguyen, a board-certified internist. “Concurrent symptoms like weight loss or dehydration necessitate same-day assessment.”
Advanced imaging techniques detect foreign bodies or tumors missed by physical exams. Fecal tests rule out parasites, while blood work screens for systemic diseases. Timely diagnosis prevents progression to life-threatening conditions like septic peritonitis.
Conclusion
Persistent gastric distress in felines demands a dual approach of observation and action. Research indicates that yellow liquid expulsion often stems from prolonged fasting or undiagnosed conditions like inflammatory bowel disease. A 2023 Veterinary Medicine International study found structured feeding schedules reduced episodes by 58% in predisposed animals.
Owners should note recurring patterns and accompanying symptoms. Behavioral changes such as reduced grooming or appetite shifts frequently precede clinical deterioration. Immediate veterinary assessment becomes crucial when incidents exceed twice weekly or show blood traces.
Preventive strategies combine dietary adjustments with routine care. Splitting meals into smaller portions maintains digestive activity, while regular grooming minimizes hairball risks. As Cornell University’s Feline Health Center advises: “Proactive monitoring paired with professional guidance offers the best outcomes for chronic cases.”
Evidence-based interventions underscore the importance of tailored solutions. While home management addresses mild scenarios, persistent issues require diagnostic imaging and specialized treatment plans. Balancing preventive measures with timely medical care remains key to safeguarding feline well-being.














