Ever stood up after a long Netflix binge and felt like your legs were filled with cement? That’s your veins sending an SOS. Chronic venous insufficiency affects a staggering 40% of Americans—more than the population of California and Texas combined—yet most people dismiss those achy, swollen legs as just another sign of aging.
Think of your leg veins as an elevator struggling to lift blood back to your heart. When that system breaks down, blood pools in your lower extremities like rush-hour traffic with nowhere to go. The result? A cascade of uncomfortable symptoms that can seriously cramp your style—and your health.
Overview of Chronic Venous Insufficiency (CVI)
Ever wondered why your legs feel heavy and swollen after standing all day? It might be chronic venous insufficiency (CVI), a condition where your leg veins struggle to send blood back to your heart. Think of it like a broken escalator – instead of moving upward, blood pools in your legs, creating pressure that can be quite the party pooper.
CVI affects a whopping 40% of Americans – that’s more people than those who watch the Super Bowl! Women get the short end of the stick here, especially after multiple pregnancies. And if you’re middle-aged or older, your odds go up too.
The culprit? Faulty valves in your veins that just can’t do their one job: preventing blood backflow.
Common Symptoms of CVI
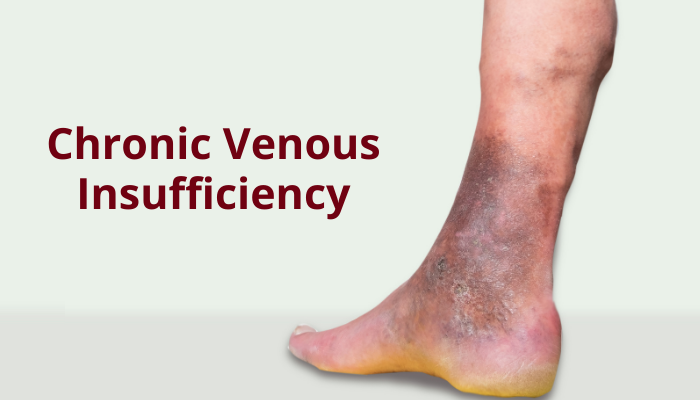
When your leg veins fail at their job, they don’t suffer in silence – they complain loudly through your body. The classic signs? A dull, heavy aching in your legs that gets worse when you stand but magically improves when you prop your feet up. Most folks notice swelling, especially around the ankles, that worsens throughout the day.
Those twisted, bulging varicose veins aren’t just a cosmetic nuisance – they’re your body’s distress signal. Your skin might join the protest too, turning reddish-brown near your ankles or becoming itchy and irritated.
In severe cases, open sores called venous ulcers can form – stubborn wounds that heal slower than a snail on vacation. Some people even experience strange sensations like tingling or an irresistible urge to move their legs at night.
Individuals Most at Risk for CVI
Looking for someone who’s likely to develop venous problems? Check the family photo album first. CVI often runs in families—thanks a lot, genetics! Women pull the short straw here too, with hormonal changes putting them at higher risk than men.
Had a blood clot in your leg before? That deep vein thrombosis (DVT) can damage valves and set you up for CVI down the road. And if you’re carrying extra pounds, those leg veins feel the pressure—literally. Your risk jumps significantly with obesity.
Pregnant women face a temporary perfect storm: hormonal changes, increased blood volume, and a growing uterus putting pressure on veins. Tall folks also face higher risks (more vertical distance for blood to travel), as do those who spend their days sitting at desks or standing on assembly lines. The human body just wasn’t built for that kind of stillness!
Causes of Chronic Venous Insufficiency
Ever looked at a leaky faucet and thought, “That’s basically what’s happening in my legs”? The main culprit behind CVI is faulty valves—tiny one-way doors inside your veins that should snap shut after blood passes through. When they fail, blood trickles backward and pools instead of flowing upward to your heart.
Some folks are born with naturally weak valves—thanks for nothing, genetics! Others develop problems after a blood clot damages the valves. That’s why a history of deep vein thrombosis (DVT) puts you in the danger zone for venous issues later.
Your lifestyle plays a huge role too. Sitting or standing for hours on end makes your veins work overtime against gravity. Smoking constricts blood vessels, while extra weight puts additional pressure on leg veins. It’s like asking them to push a boulder uphill while wearing flip-flops—not exactly setting them up for success!
Complications of Chronic Venous Insufficiency
When blood pools in your legs for too long, it’s like leaving standing water in your basement—nothing good comes from it. The most feared complication? Venous ulcers. These stubborn, open sores typically form near the ankles and can take months or even years to heal. They’re not just painful—they’re downright persistent party crashers.
Your skin throws a fit too. Stasis dermatitis shows up as red, itchy patches that can become scaly and weepy. Over time, your skin might thicken and harden (a condition doctors call lipodermatosclerosis), feeling like leather rather than your normal skin.
Those bulging varicose veins aren’t just ugly—they’re fragile! One wrong bump and you could experience bleeding that seems way too dramatic for such a small injury. And let’s not forget about infection risk—those compromised tissues are practically rolling out the welcome mat for bacteria.
Diagnosis of CVI
If you suspect your legs are staging a venous rebellion, it’s time to see a doctor. They’ll start with a good old-fashioned physical exam, checking for swelling, skin changes, and those telltale varicose veins. But the real MVP of CVI diagnosis is the duplex ultrasound—a painless test that uses sound waves to create images of your veins and measure blood flow.
Think of it as giving your veins their own reality show! The ultrasound reveals if your valves are slacking on the job and shows any blockages that might be causing trouble. Best part? It’s non-invasive—no needles, no pain, just a little cool gel on your legs.
Some doctors might order a venogram (using dye and X-rays) or magnetic resonance venography for complex cases, especially to rule out other leg pain culprits like peripheral artery disease.
Treatment Options for Chronic Venous Insufficiency
Treating CVI is like waging a multi-front war against gravity. The good news? You’ve got options that don’t involve rocket science.
First line of defense: compression stockings. These tight-fitting socks squeeze your legs, helping blood flow upward instead of pooling. They’re not exactly fashion statements, but they work wonders when worn daily. For mild cases, knee-high versions might do the trick, while more serious situations call for thigh-highs.
When compression isn’t enough, doctors might suggest more active approaches. Sclerotherapy involves injecting a solution that scars problematic veins, forcing blood to reroute through healthier channels. For larger veins, radiofrequency or laser ablation heats and seals the troublemakers shut—all through a tiny needle prick!
The old-school approach? Vein stripping, where surgeons remove the faulty vein entirely. It sounds medieval, but sometimes it’s the best option for severe cases. Modern techniques make it much less painful than it sounds.
Your everyday habits matter too. Regular walking activates your calf muscles, which act like mini-pumps pushing blood upward. Losing weight takes pressure off those overworked veins, while elevating your legs above heart level whenever possible gives them a well-deserved break from fighting gravity.
When to Consult a Medical Professional
Don’t wait until your legs are crying for help! If your varicose veins are getting bigger or more painful, that’s your body waving a red flag. Persistent swelling that doesn’t improve after a night’s rest? Time to make that appointment.
Skin changes around your ankles – like redness, hardening, or that brownish discoloration – aren’t just cosmetic concerns. They’re your veins’ distress signals! And if you spot an open sore that’s taking its sweet time healing (especially near your ankle), run (don’t walk) to the doctor. These venous ulcers can lead to nasty infections if ignored.
Sudden, severe leg pain or swelling could signal a blood clot – a medical emergency that needs immediate attention. Remember, poor circulation issues get worse over time, not better!
When Your Veins Need a Helping Hand
Living with chronic venous insufficiency doesn’t mean surrendering to a life of discomfort. From compression stockings that give your veins a boost to surgical interventions that reroute blood flow, treatments exist for every stage of this condition. The key is catching it early, before those minor annoyances evolve into serious complications.
Remember, those legs carry you through life—they deserve better than to suffer in silence. If you’re experiencing persistent swelling, skin changes, or varicose veins that seem to have their own zip code, don’t wait for them to improve on their own. Your future self—with happier, healthier legs—will thank you for taking action today.